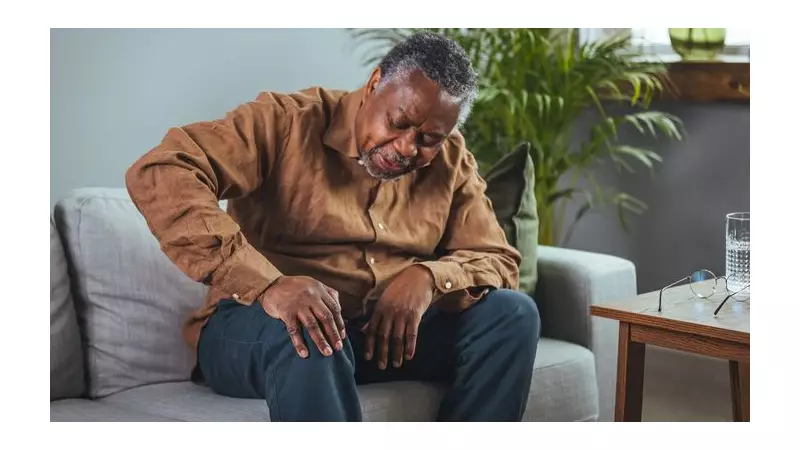
As temperatures plummet across the UK, a familiar and unwelcome guest arrives for many: increased joint stiffness and pain. That persistent tightness in knees, fingers, and hips is far from a simple coincidence. Leading health specialists reveal the fascinating biological mechanisms behind this seasonal discomfort and provide actionable solutions to help you stay mobile.
The Science Behind Seasonal Stiffness
Rehabilitation specialist Jon Taberner from Nuffield Health explains that while all body parts can be affected, we often feel it most in "joints with complex bone structures furthest away from our core body". For those already managing worn or damaged joints, the cold can significantly amplify these existing sensations.
One primary reason is our body's natural protective response. In cold conditions, heat is diverted from our limbs to protect vital organs. Taberner notes that "this results in less blood flow to our joints", leading to poorer lubrication and a notable increase in pain. This effect is often more pronounced with age and can be worse for those with a history of manual labour or conditions like diabetes.
London-based physiotherapist Ben Lombard highlights another key factor: our tendency to be less active. "Reduced activity can lead to reduced lubrication and muscle weakness," he states. The synovial membrane, which produces joint-lubricating fluid, becomes less efficient in the cold, making the fluid thicker and less effective.
How Weather and Pressure Play a Role
The atmosphere itself contributes to the ache. During winter storms, barometric pressure often drops. Lombard points out that this shift can cause "muscles and tendons to create more pressure on the joints," resulting in that deep-seated, seasonal pain many people report.
Practical Strategies to Ease Winter Joint Discomfort
Experts agree that proactive measures are far more effective than simply masking pain. Here are their top, evidence-based tips for maintaining comfort and mobility.
1. Layer Up for Core Warmth: Lombard suggests that "wearing thermals and layers, as simple as it sounds, can be quite useful." Keeping your core body temperature stable helps maintain better blood flow to your extremities.
2. Apply Targeted Heat: Using a hot water bottle or a microwaveable heat pack on stiff areas can manually stimulate blood circulation and help relax tight muscles, providing direct relief.
3. Prioritise Hydration: Since synovial fluid is influenced by your body's hydration levels, Lombard confirms that "hydration generally would certainly help keep things more mobile and flexible." Drinking enough water is a simple yet powerful tool.
4. Keep Gently Moving: Regular, gentle motion is crucial. Taberner explains that exercise "increases blood flow to the joints you are moving" and helps warm the entire body, triggering the release of natural lubricants.
While over-the-counter painkillers can offer temporary relief, Taberner insists they do not solve the "overarching issues" and should be combined with preventative measures like strength training. He strongly emphasises the importance of seeking professional advice: "contact your medical professional if the pain is new or noticeably more severe", or if you notice any accompanying redness and swelling.
Before embarking on any new fitness programme to combat stiffness, always consult your GP or a qualified physiotherapist. They can ensure the movements are safe for your specific needs and help you build an effective, enjoyable routine for long-term joint health.